I had been in labor for 51 hours—slowly realizing I was headed toward a cesarean section—when the on-call obstetrician came to my bedside. "I'm about to head out," she told me gently, "but the doctor coming on shift, Dr. K, is incredible. I'll send her in right away."
To her surprise, I groaned. "I've met her," I retorted through clenched teeth. "She processed my miscarriage…" I stopped to think, "almost exactly one year ago. To the day."
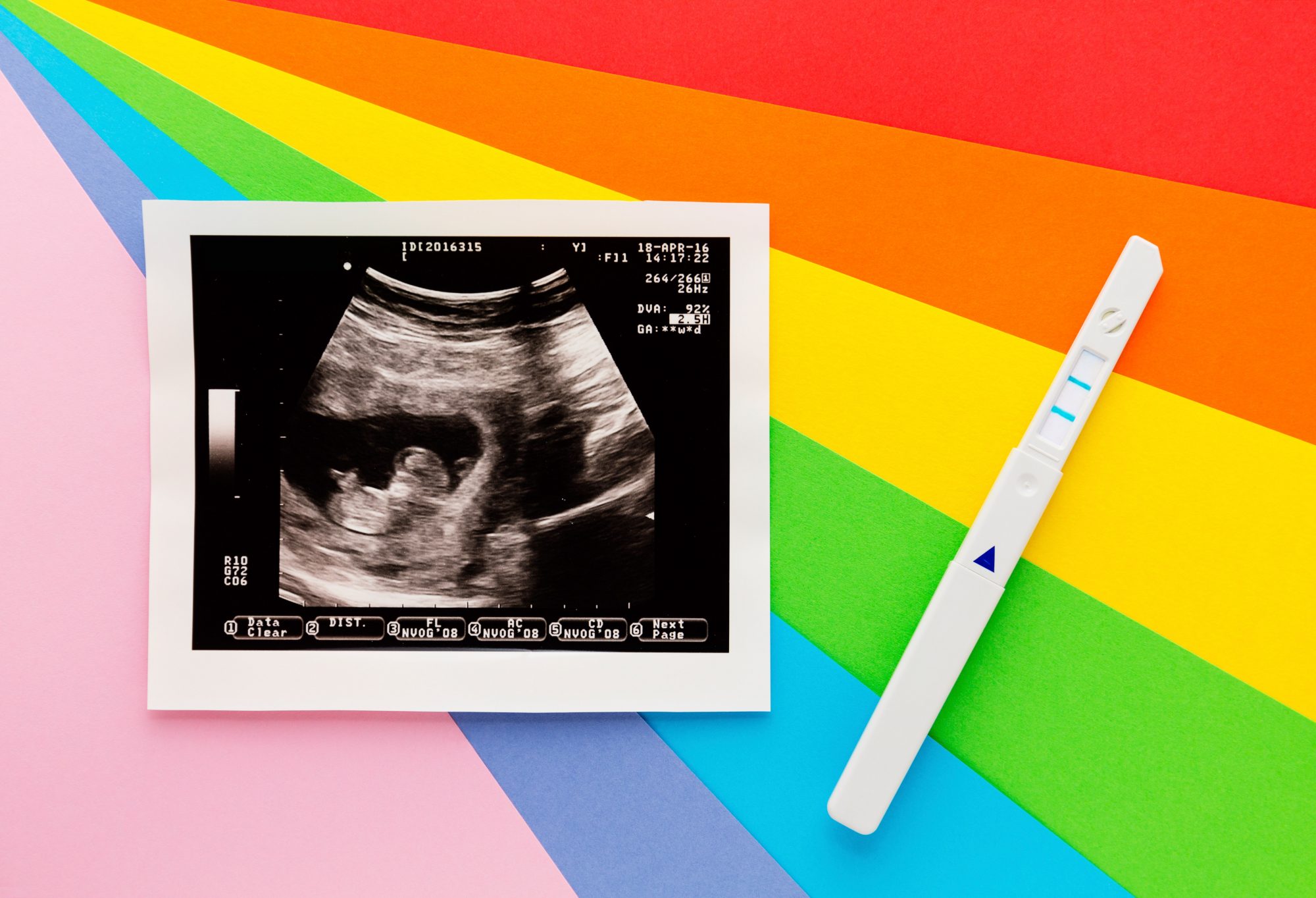
I'd spent the entirety of my second pregnancy trying not to think about my first. Dr. K, as I'll call her here, had been on call when I needed dilation and evacuation (D&E) when I was 13 weeks pregnant in 2019. She was eminently professional and compassionate during my miscarriage. I never wanted to see her again. During this pregnancy, I'd checked every appointment to make sure I wouldn't have to. I'd even debated going to a different hospital to deliver, just in case.
Now this doctor who I've labeled "unlucky" was literally staring me in the face in the delivery room.
Am I about to lose another baby? I wondered.
Transferring Grief: When Patients Cope Through Avoidance
If this sounds familiar—an overwhelming need to avoid the circumstances and people involved with a loss—you're not alone. Grieving patients commonly label perfectly capable doctors who deliver bad news or perform painful termination procedures as "tainted" or "jinxed"—an unfair classification, but one that speaks to the pain they feel.
Steve Rad, M.D., FACOG, is a renowned maternal-fetal medicine perinatologist specializing in advanced ultrasound, fetal abnormalities, and high-risk pregnancies. He experiences this every day. "I see patients where I diagnose a miscarriage and they disappear. I get really hurt—what did I do? How could they leave? Did I say something wrong?" he says. But then, by contrast, he gets a lot of second opinions and becomes the doctor who helps a patient through a loss and with a future pregnancy.
In other words, when a patient receives traumatic information, it's an easy (and common) psychological response to make an association between the messenger and the message—and have an avoidant response as a result. This is particularly true if the medical professional had a bad bedside manner, to be sure, but it's more representative of how uniquely upsetting the event is.
"The loss of a baby is completely wrong on so many levels. Where there should be life there is death," says Janet Jaffe, Ph.D., co-founder and director of the Center for Reproductive Psychology in San Diego, California, and co-author of Unsung Lullabies: Understanding and Coping with Infertility. "And it's out of order: as a society we expect grandparents to predecease parents to predecease us. It's a pain unlike any other—ever. It goes right to our definition of ourselves."
Why Negative Associations Around Pregnancy Loss Develop
Between 10 to 20 percent of pregnancies end in miscarriage, but this number is likely underreported. Not only that, but Dr. Rad explains that in his experience "we have no clue why it happened. Even when we check patients' genetics, blood tests, ultrasounds, 99 percent of the time we find nothing." So the truth is that there is no one to blame, but the grief remains.
"The trauma we see from miscarriage is worse than the women we see who have the most high-risk pregnancies," he says. "We get several calls a day. The high-risk pregnancies get referred to me, but women who have had miscarriages are calling directly believing they're high risk."
Patients may go to extreme lengths searching for the things they must have done to cause the pregnancy loss, in order to take back this illusory control. Did they exercise too strenuously? Did they inhale a toxic chemical? Did they accidentally have too much sugar?
Since people often do not share pregnancy news in the first few weeks, those around them may not even know they're grieving. When they do share, the messaging can sometimes be traumatizing—from friends, family, or professionals. "We are told, perhaps indirectly, to get over it. 'You're young, don't let this affect your life. You'll have another'—as if you could replace a baby. Women are given the message that you're not supposed to feel the way you feel and that you are wrong to have these feelings," says Dr. Jaffe.
She sees women who are coming to therapy for the first time, traumatized not just by the loss but by the way in which the news was delivered. "It's not that doctors don't have feelings about these losses, they do, but in some ways it's just another day at the office. But for women receiving the news, it's the worst thing she could hear."
So, the patient might make an association between the messenger and the message. Somehow, the doctor must have done something, because the truth—that this was just a random life event—is unbearable. Whether through superstition or trauma (or both), patients resolve not to do what they did the first time around, which may lead to them changing doctors.
How Can Doctors and Medical Professionals Help Patients Through a Miscarriage?
Medical professionals aren't necessarily trained in trauma or delivering bad news (the ultrasound tech stopped talking to me and wouldn't look me in the eye as soon as she realized what she was looking at—so it's not just the doctor who can accidentally traumatize). They might have to put in extra work to learn how to communicate as compassionately as possible.
Dr. Rad lays out his approach: "If I ever have to tell a patient they've had a miscarriage, I stop and say: 'This is not your fault. You didn't bend down too much. You didn't do an exercise that was off. You didn't take too hot of a shower. It wasn't that you were stressed or got in a fight with your partner. It wasn't because your boss said something, or you ate spicy food.'"
"I come up with extreme things to drive the point home that it's not their fault, their body isn't broken, it doesn't mean you can't get pregnant again. Unfortunately, I think at that point they're not listening. Once I tell them, they may not come back, but I try to tell them as much as I can."
Doctors can also try and help their patients talk through their fear, lest they carry it with them through the next pregnancy. Doctors can refer patients to a therapist. Rainbow clinics, even though they don't exist everywhere, are specifically tailored to help would-be birthing parents with their unique loss(es) and make a gentle caring environment if they want to get pregnant again. Patients who have had a negative experience with a doctor can look for these clinics, or seek out a provider who understands how to communicate loss in this way.
How Can Patients Address Their Feelings?
Before making any decisions about their care, patients need to process what happened. In my case, I flip-flopped between anger and guilt, but my skilled trauma therapist helped me see that both were untrue. Dr. Jaffe recommends speaking with specialists trained with the American Society of Reproductive Medicine (ASRM), because they already speak the language of loss, infertility, and pain.
"It's so important for a person to tell their reproductive story, the trauma of what happened, and then also talk about the earlier story: what they thought would happen. How did things go so 'wrong'?" she says. "Within that there are assumptions about pregnancy like: I'm strong, I thought it would be easy. These are core beliefs that are now shattered. It's essential [for therapists] to talk about these things…to make the experience real, to sit with them and let them remember what happened. That validation is critical."
There were mantras I could tell myself to stay present. Knowing that the embryo came from me, but was not me, was helpful. So was knowing that I am healthy and I had a miscarriage—that both can be true at the same time. Not blaming the doctor started by not blaming myself. And yet, still having these feelings throughout any subsequent pregnancy (as I did) is common. Adds Dr. Jaffe, "When people have had a loss, they anticipate having another loss. I've never met anyone who hasn't had anxiety during a subsequent pregnancy."
Keeping the Same Doctor Might Offer Closure
There's also value in honoring the loss: unlike when a family member dies, there are no stories or memories beyond an ultrasound, doctor's visit, or painful procedure. Talking to people whom you trust, and giving voice to the pain—including to your medical provider—can be useful. In fact, says Dr. Jaffe, patients who stay with their doctors who processed their miscarriages can sometimes feel that the doctor knows their pain and history. The concept of explaining what happened to a new clinician feels unbearable. When a clinician and patient bond and trust each other, it can make the experience easier.
So, even though you are not bound to do anything you don't want to, you might heal by continuing to go to the same doctor. At least, that's what happened to me.
Dr. K came in, with the sweet gentleness that had so grated on my nerves when we first met, and told me it was good to see me again. Then, she explained what the C-section would look like. "In 15 minutes, you're going to be parents!" she told us. The operating room was filled with female doctors, nurses, and technicians, and the vibe was warm and joyful: Dr. K chatted throughout, letting me know what she was doing (but avoiding some of the scarier details so I wouldn't freak out).
As soon as my baby made it into the world, she let out an ear-splitting squawk at being so unceremoniously evicted. Everyone stopped what they were doing to turn and look at her. Dr. K said, "Wow. I've never heard that shriek before." Everyone in the room laughed, including me, as I brushed away tears.
I had a healthy baby—and some closure to go along with it.